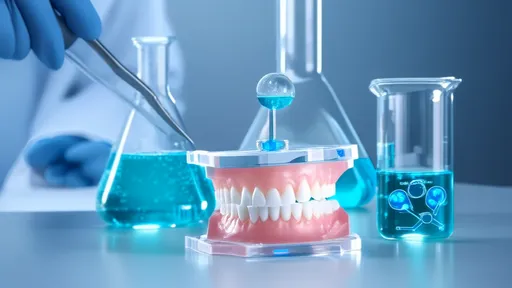
The field of dentistry has long grappled with the challenge of biofilm formation on dental materials, a persistent issue that contributes to oral diseases and implant failures. Biofilms, which are complex communities of microorganisms encased in a protective extracellular matrix, pose significant risks to both natural and artificial dental structures. Recent advancements in biofilm inhibition technologies are revolutionizing how dental professionals approach prevention and treatment, offering promising solutions to enhance patient outcomes.
One of the most groundbreaking developments in this area is the incorporation of antimicrobial agents directly into dental materials. Researchers have successfully integrated compounds such as silver nanoparticles, chlorhexidine, and quaternary ammonium salts into resins, cements, and composites. These agents work by disrupting bacterial cell membranes or interfering with metabolic processes, effectively reducing biofilm formation without compromising the material's structural integrity. Studies have shown that these modified materials can significantly decrease bacterial adhesion and proliferation, particularly against common oral pathogens like Streptococcus mutans and Porphyromonas gingivalis.
Surface modification techniques have emerged as another powerful strategy in biofilm prevention. By altering the topography or chemistry of dental material surfaces at the nanoscale level, scientists can create surfaces that are inherently resistant to bacterial colonization. Methods such as plasma treatment, laser texturing, and the application of superhydrophobic coatings have demonstrated remarkable success in making surfaces less hospitable to microbial attachment. These approaches are particularly valuable for dental implants and prosthetics, where long-term biofilm resistance is crucial for clinical success.
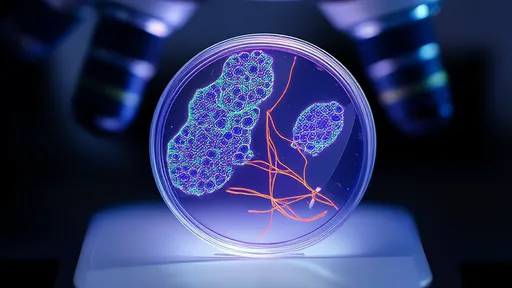
The development of smart, responsive dental materials represents a paradigm shift in biofilm control. These innovative materials can detect changes in their microenvironment, such as pH shifts or enzymatic activity associated with bacterial growth, and respond by releasing antimicrobial agents or altering their surface properties. For instance, pH-sensitive polymers embedded in restorative materials can release calcium and phosphate ions when acidic conditions develop, simultaneously remineralizing tooth structure and creating an environment less conducive to bacterial survival. Such dynamic systems offer the advantage of targeted, on-demand action while minimizing unnecessary exposure to antimicrobials.
Natural compounds are gaining attention as potential alternatives to synthetic antimicrobials in dental applications. Plant-derived substances like polyphenols, essential oils, and antimicrobial peptides exhibit promising biofilm-inhibiting properties with potentially fewer side effects than traditional agents. Researchers are exploring ways to incorporate these bioactive molecules into dental adhesives, liners, and even temporary restorative materials. The combination of natural antimicrobials with conventional materials could provide a more biocompatible approach to biofilm management, particularly for patients with sensitivities to synthetic compounds.
Photodynamic therapy (PDT) has shown considerable promise as an adjunctive biofilm control method for dental applications. This technique involves the use of light-sensitive compounds that, when activated by specific wavelengths of light, generate reactive oxygen species capable of destroying bacterial cells. Dental materials incorporating photosensitizers or designed to work in conjunction with PDT protocols offer a non-invasive way to control biofilm formation, especially in hard-to-reach areas around restorations and orthodontic appliances. The precision of this method allows for targeted treatment while preserving surrounding healthy tissues.
Despite these technological advances, challenges remain in translating laboratory successes to clinical practice. The long-term stability of antimicrobial agents within dental materials, potential effects on mechanical properties, and concerns about microbial resistance necessitate ongoing research. Furthermore, regulatory approvals and cost considerations play significant roles in determining which technologies will ultimately reach dental practices. Collaborative efforts between material scientists, microbiologists, and clinicians are essential to develop solutions that are not only effective against biofilms but also practical for routine dental use.
Looking ahead, the integration of multiple biofilm-inhibition strategies may offer the most comprehensive approach. Combining surface modifications with controlled-release antimicrobial systems and smart responsive technologies could create synergistic effects that surpass the capabilities of individual methods. As our understanding of oral biofilms deepens and material science continues to advance, the next generation of dental materials promises to provide unprecedented levels of protection against microbial colonization, ultimately leading to more durable restorations and improved oral health outcomes for patients worldwide.

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025